Crohn’s Disease Treatments: Medication vs Lifestyle Changes sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset.
The discussion dives into the intricacies of managing Crohn’s disease through a balanced approach of medication and lifestyle changes, shedding light on effective strategies for individuals dealing with this condition.
Medication for Crohn’s Disease
When it comes to managing Crohn’s disease, medication plays a crucial role in controlling symptoms and preventing flare-ups. Several types of medications are commonly prescribed to individuals with Crohn’s disease, each with its own mechanism of action and effectiveness.
Common Medications for Crohn’s Disease
- Corticosteroids: These medications help reduce inflammation in the digestive tract and are often used during flare-ups.
- Immunomodulators: Drugs like azathioprine and methotrexate work by suppressing the immune system to reduce inflammation.
- Biologics: These medications target specific proteins in the body to reduce inflammation and are often used in moderate to severe cases of Crohn’s disease.
- Aminosalicylates: These medications help reduce inflammation in the lining of the intestines and are often used for mild cases of Crohn’s disease.
Mechanism of Action
Each type of medication for Crohn’s disease works in a different way to manage symptoms and reduce inflammation. Corticosteroids, for example, mimic the effects of cortisol in the body to suppress inflammation. Immunomodulators work by targeting the immune system to reduce inflammation, while biologics target specific proteins to block the inflammatory response.
Aminosalicylates, on the other hand, reduce inflammation in the intestines by inhibiting certain enzymes.
Effectiveness of Different Medications
The effectiveness of medications for Crohn’s disease can vary depending on the individual and the severity of the condition. Biologics are often considered more effective in treating moderate to severe cases of Crohn’s disease, while aminosalicylates may be sufficient for mild cases.
It is essential for healthcare providers to tailor treatment plans to each patient’s specific needs and monitor their response to medication to ensure the best outcomes.
Lifestyle Changes for Crohn’s Disease
Managing Crohn’s disease involves not only medication but also making significant lifestyle changes to improve symptoms and overall quality of life.
Diet Modifications
Diet plays a crucial role in managing Crohn’s disease symptoms. Here are some examples of diet modifications that can help:
- Avoiding trigger foods such as spicy foods, dairy, and high-fiber foods that can worsen symptoms.
- Opting for a low-residue diet to reduce bowel movements and inflammation.
- Incorporating more easily digestible foods like well-cooked vegetables, lean proteins, and refined grains.
Exercise for Quality of Life
Regular exercise can have a positive impact on individuals with Crohn’s disease by improving overall health and quality of life. Here’s how exercise can help:
- Reducing inflammation and boosting the immune system.
- Alleviating stress and anxiety, which are common triggers for Crohn’s disease flares.
- Promoting better digestion and bowel regularity.
Combination Therapy
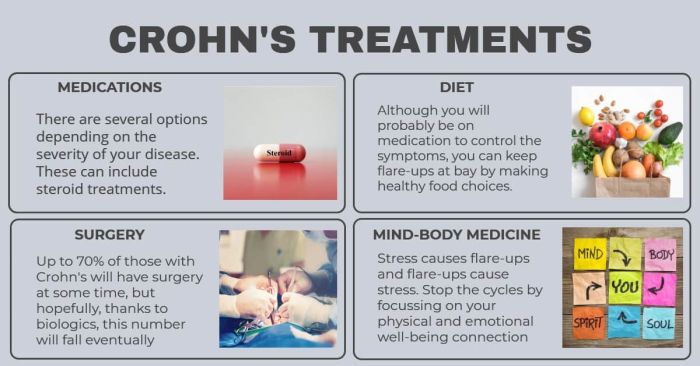
Combination therapy, which involves a mix of medication and lifestyle changes, has shown great promise in effectively managing Crohn’s disease. By combining these two approaches, patients can experience better symptom control, reduced inflammation, and improved overall quality of life.
Benefits of Combination Therapy
- Enhanced symptom relief: Medications can help target inflammation internally, while lifestyle changes such as diet modifications and stress management techniques can further alleviate symptoms.
- Reduced flare-ups: The combined approach can help reduce the frequency and severity of disease flare-ups, leading to longer periods of remission.
- Improved overall health: Incorporating lifestyle changes like regular exercise and adequate sleep alongside medication can promote better overall health and well-being.
Successful Treatment Plans
- Example 1: A patient with Crohn’s disease may be prescribed anti-inflammatory medications to target inflammation, along with dietary changes to avoid trigger foods and promote gut health.
- Example 2: Another patient may benefit from a combination of immunosuppressants to control the immune response, along with stress-reducing activities like yoga or meditation.
Determining the Best Combination Therapy
- Healthcare professionals typically assess each patient individually to determine the most suitable combination therapy based on the severity of their symptoms, medical history, lifestyle factors, and treatment goals.
- Factors such as medication side effects, patient preferences, and response to initial treatments are taken into consideration when creating a personalized treatment plan.
Potential Side Effects
Crohn’s disease medications can come with various side effects that may affect the patient’s quality of life. Some common side effects include nausea, vomiting, diarrhea, abdominal pain, headaches, and fatigue. These side effects can be challenging to manage and may lead to non-compliance with the prescribed treatment.Lifestyle changes play a crucial role in mitigating the side effects associated with Crohn’s disease medications.
For example, maintaining a healthy diet low in trigger foods, staying hydrated, getting regular exercise, managing stress levels, and getting enough rest can help reduce the severity of gastrointestinal symptoms and improve overall well-being.Monitoring side effects is essential when undergoing treatment for Crohn’s disease.
Patients should communicate openly with their healthcare providers about any side effects they experience. Regular check-ups and blood tests can help detect any potential issues early on and allow for timely adjustments to the treatment plan. It is important for patients to be proactive in managing their symptoms and seeking support when needed.
Final Wrap-Up
In conclusion, the blend of medication and lifestyle adjustments presents a comprehensive approach to managing Crohn’s disease, emphasizing the importance of personalized treatment plans tailored to each individual’s needs. This holistic perspective offers hope and empowerment to those navigating the challenges of living with this chronic condition.
FAQ Guide
Can lifestyle changes alone cure Crohn’s disease?
While lifestyle modifications can help manage symptoms, Crohn’s disease typically requires a combination of medication and lifestyle adjustments for effective treatment.
Are there any specific diets recommended for individuals with Crohn’s disease?
Certain diets like low-residue or low-FODMAP diets may be beneficial for some individuals with Crohn’s disease, but it’s essential to consult with a healthcare provider for personalized dietary recommendations.
How can exercise impact Crohn’s disease management?
Regular exercise can improve overall health and quality of life for individuals with Crohn’s disease by boosting immunity, reducing inflammation, and promoting mental well-being.
What are common side effects of Crohn’s disease medications?
Side effects can vary depending on the medication but may include nausea, diarrhea, fatigue, and increased risk of infections. Monitoring for these side effects is crucial during treatment.